When we wake in the morning and hop on our two feet to go on about our everyday tasks, we forget this can change in one day.
Most of us take our health for granted, especially when we’re young. But a single car accident or a sudden fall can bring major trauma to a person’s once-healthy body.
That’s why being a professional occupational therapist can flip a client’s life from a negative to a more positive journey where they can expect to get back to their past lives sooner than later.
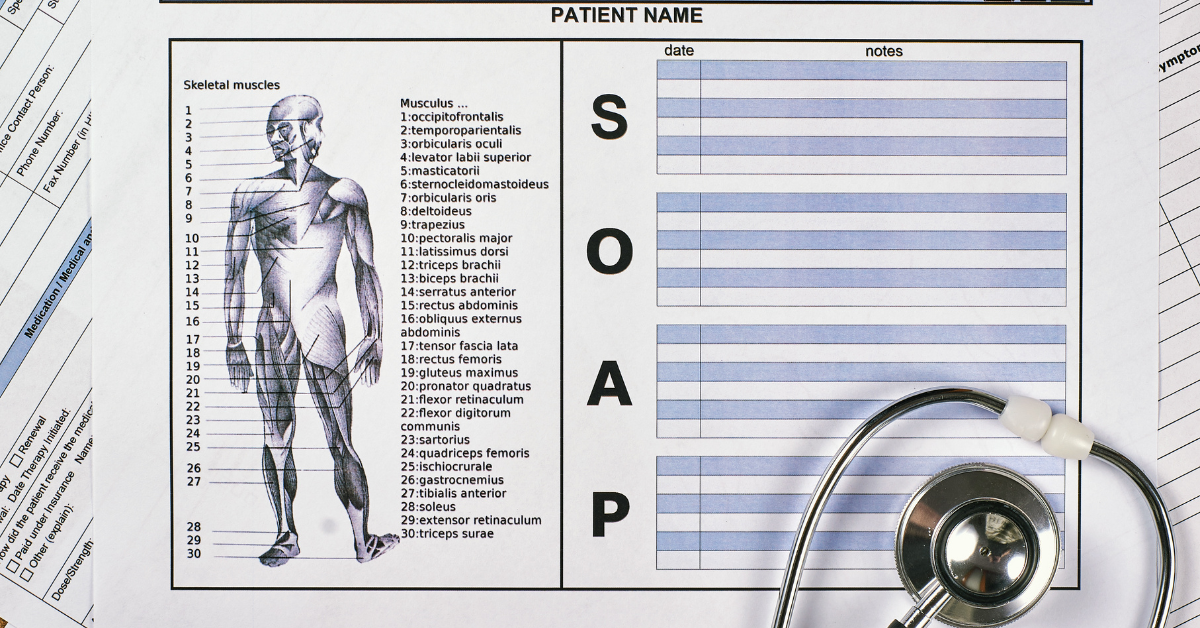
And as an occupational therapist, your SOAP notes play a pivotal role in documenting your patient’s progress, guiding treatment plans, and fostering effective communication with other healthcare professionals.
In this unique exploration, we’ll delve into the art of the well-structured and insightful SOAP note format.
Discover essential tips, real-life examples, and practical strategies to write SOAP notes and elevate your clinical documentation skills, ensuring optimal care and improved outcomes for your patients.
Whether you’re a seasoned OT practitioner seeking refinement or a newcomer eager to master the craft, this guide will equip you with the right tools to excel in the art of Occupational Therapy SOAP note writing.
What Are Occupational Therapy SOAP Notes?
Occupational Therapy (OT) SOAP treatment notes are a structured and organized method of clinical documentation used by occupational therapists to record patient information, assessments, interventions, and treatment plans.
The SOAP format ensures consistency, clarity, and a comprehensive approach to patient care.
Let’s break down each component of an OT SOAP note-taking with examples:
S – Subjective
In the subjective data section, the therapist records information provided by the patient or caregiver about their feelings, perceptions, and concerns during the occupational therapy session. This includes the patient’s chief complaints, subjective experiences, and any relevant personal history.
Example: “Patient reports difficulty with dressing independently due to limited range of motion in the right shoulder following a recent injury.”
O – Objective
The objective section contains measurable and observable data gathered by the occupational therapist during the evaluation or treatment session. This may include results from standardized assessments, physical measurements, and specific observations.
Example: “Occupational therapist performed goniometric measurements, revealing a 20% decrease in the right shoulder’s range of motion compared to the left shoulder.”
A – Assessment
In the assessment section, the occupational therapist interprets the subjective and objective information to identify the patient’s strengths, limitations, and potential problem areas. This is where the therapist formulates a clinical impression or diagnosis based on their evaluation and is mainly related to writing a treatment note.
Example: “Based on the patient’s report and objective findings, the occupational therapist assesses the patient with a right shoulder impingement syndrome, resulting in decreased functional independence in dressing activities.”
P – Plan
The plan section outlines the occupational therapist’s proposed interventions and treatment goals. It includes specific strategies, therapeutic activities, and expected outcomes to address the identified issues.
Example: The occupational therapist will implement a therapeutic exercise program to improve the range of motion in the right shoulder. The patient will also receive training in adaptive dressing techniques and compensatory strategies to promote independence.
7 Tips on Perfecting Your Occupational Therapy SOAP Notes
Perfecting your Occupational Therapy SOAP notes is essential for effective patient care and communication with other healthcare professionals.
Here are seven valuable tips to help you refine your documentation skills:
Be Clear and Concise
Use clear and concise language in your SOAP notes to convey essential information effectively. Avoid unnecessary jargon or ambiguous terms that could lead to misinterpretation.
Include Functional Goals
Incorporate specific and measurable functional goals in the “Plan” section of your SOAP notes. Clearly outline the objectives you aim to achieve with the patient, such as improving activities of daily living (ADLs), enhancing social interactions, or increasing participation in school or work-related tasks.
Example: Patient Profile: A 10-year-old child with developmental coordination disorder (DCD) struggling with handwriting.
- Plan: The occupational therapist will work on improving the child’s handwriting legibility and speed.
- Functional Goal: The patient’s functional goal is to write a complete sentence with 80% legibility and maintain a consistent speed of 8 words per minute within six weeks.
Utilize Strength-Based Language
Emphasize the patient’s strengths and capabilities throughout your SOAP notes. Recognize and highlight their achievements, even in challenging situations, to foster a positive and empowering therapeutic relationship.
Example: “The patient demonstrated excellent problem-solving skills during the activity, utilizing adaptive strategies to accomplish the task independently.”
Focus on Measurable Data
Ensure the “Objective” section includes measurable data and specific observations. Use standardized assessments and quantitative measurements whenever possible to track patient progress objectively.
Use Patient-Centered Language
Center your SOAP notes around the patient’s goals and needs. Describe interventions and treatment plans in terms that are meaningful and understandable to the patient.
Example: Patient Profile: A 65-year-old individual recovering from a stroke in s skilled nursing facility, experiencing difficulty with activities of daily living (ADLs).
- Non-Patient-Centered: “Patient requires assistance with feeding due to limited hand coordination.”
- Patient-Centered: “The individual prefers some assistance with feeding to ensure a comfortable and enjoyable dining experience.”
Document Progress Over Time
Regularly update your SOAP notes to reflect changes in the patient’s condition, progress in therapy, and adjustments to treatment goals. Track milestones and improvements to demonstrate the effectiveness of your interventions.
After several session notes, you’d use your clinical reasoning in the assessment section and take notes faster once you get used to the format.
Maintain Compliance and Clarity
Comply with legal and regulatory standards for documentation. Sign and date your SOAP notes, ensuring they are legible and complete. Use standard abbreviations and terminology to enhance clarity and consistency.
Get Better at Writing SOAP Notes and Help More Clients
Perfecting your Occupational Therapy documentation is a transformative step toward enhancing patient care and communication within the healthcare community.
By applying the tips provided while including subjective and objective data in your clinical notes, you can craft comprehensive, patient-centered, and measurable documentation that ensures optimal outcomes for your clients.
As you continue your crucial work as an occupational therapist, your dedication to crafting meaningful SOAP notes will enhance patient care and foster a more collaborative healthcare community.
Leave a Reply